While most people are singing Auld Lang Sine at midnight on January 1, those of us in the Medicare world are anxiously awaiting the first claims of the plan year to process. It is that moment of truth when plans find out if they have a member or members standing in the pharmacy unable to get their medication.
Although accurate claims processing and member access is a year-round expectation of the Centers for Medicare and Medicaid Services (CMS), plans are under even greater scrutiny by CMS and members alike at the beginning of a new plan year. In recognition of this, BluePeak has compiled the following best practices that we recommend plans implement to ensure a smooth January 1 and beyond.
Establish a Readiness Team and Escalation Process
Many plans establish a January 1 readiness cross-functional team to be available, either in person or remotely, to monitor claims activities and complaints. This team should include plan employees, as well as critical vendors, such as the Pharmacy Benefit Manager (PBM) and enrollment processor. Ensure that subject matter experts who can trouble-shoot and resolve issues are part of the team and establish a clear process for escalation. Establish short operational calls throughout the day for the first few weeks for quick checkpoints to keep lines of communication open and barriers eliminated for the problem solvers.
Communicate with Your Call Center
The call center is a plan’s first line of defense and is often the first area to be alerted in the event of issues. Ensure your call center is well staffed and aware of all the updates for the new plan year. Provide the call center with contact information on whom to notify if an issue needs to be escalated, and ensure that the communication is bi-directional. Identify a call center lead to attend operational calls to communicate any known issues to the call center team, as well as prepare for any outbound remediation calls. Perform a review of call logs to identify call trends and to research any potentially missed operational issues or misclassified grievances.
Closely Monitor Coverage Determinations, Appeals and Grievances
Access to care grievances should always be routed and addressed expeditiously, but trending such grievances in January can help identify potential issues. Look for trends in grievances that might point to underlying issues and closely monitor grievances that come through the Complaints Tracking Module (CTM). Work closely with a coverage determination lead to identify any trends with coverage determination requests and if any staff members have identified any formulary or coverage determination setup errors. Include the lead on any operational issues identified to determine how coverage determination requests may be impacted or if overrides will need to be entered until the issue has been remediated.
Rejected Claims Review
CMS expects plans to review denied claims daily; however, at the start of the plan year, denied claims review may be as frequent as hourly. In addition to the typical items reviewed during rejected claims, extra attention should be dedicated to validating that formulary changes are processing as anticipated and that new and returning members are receiving transition supplies. Don’t rely solely on your PBM for rejected claims monitoring. While their review is critical, you must also demonstrate to CMS that you are managing the process.
Paid Claims Review
While rejected claims have been a major focus in past years, paid claims review is equally as important as rejected claims review in detecting potential set-up issues. These claims should also be reviewed daily in the early days of January to validate claims and the formulary is being applied correctly.
Retrospective Data Validation
Plans should be creating and validating their CMS universes monthly and year-round. It is particularly critical to run universes at the start of the new plan year to ensure the logic remains accurate and reliable after the new plan year configuration. Ensuring complete and accurate universes will ensure you are ready in the event you are selected for a Transition Monitoring Program Audit (TMPA), Formulary Administration Audit (FAA) or an Appeal Timeliness Monitoring review.
BluePeak Can Help
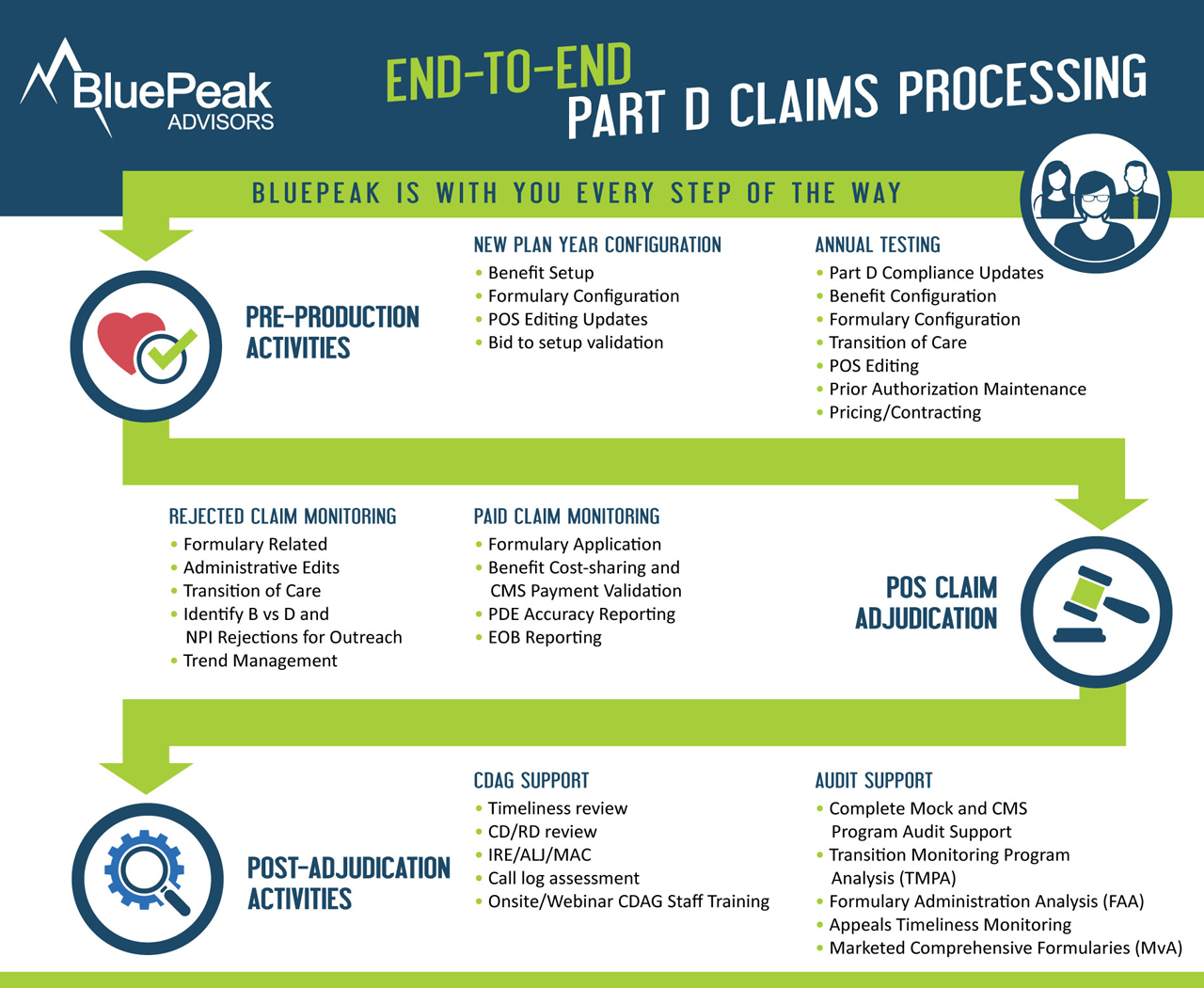
As you prepare for 2018 success, BluePeak Part D experts can help. We offer claims monitoring and testing, universe monitoring, and audit readiness and support. Cheers to the new year and another chance to get it right.

